Antimicrobial resistance (AMR) is a major global public health threat and growing in Canada. Overuse and misuse of antibiotics and other antimicrobials is increasing drug-resistance in microbes that spread among and between humans, animals and plants. AMR is making infectious diseases harder or impossible to treat and that affects us all. World AMR Awareness Week (WAAW), held November 18 to 24, is a time to build awareness and encourage action.
NEW WEBINAR SERIES
CAN AMS! webinars share examples of leading Antimicrobial Stewardship interventions and inspire what CAN be done to slow AMR.
REGISTER HERE for the upcoming webinar
More on the series

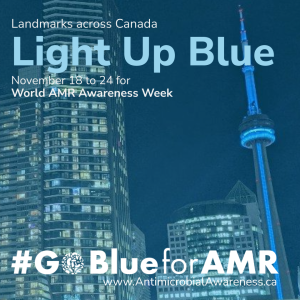
THE 2023 CAMPAIGN

#GoBlueforAMR to raise awareness and spark action!
Antimicrobial resistance (AMR) is one of the top global health threats, yet most Canadians don’t recognize the harm it is causing. #GoBlueforAMR is a Canada-wide colour campaign to increase the visibility of AMR and spark action. Follow campaign progress as landmarks and public buildings across Canada (Google map of locations), including Canada Place and the CN Tower, sign on and light up blue for the close of World AMR Awareness Week (Nov 18-24).
Help share the campaign!
You can help build awareness of AMR by sharing GoBlue messages and this website of resources with friends, family, and colleagues.
Select an image to download and post alongside the suggested messaging found below.
Suggested message#1.
#AMR is a top ten public health threat. Help shine a light on this crisis and spread awareness about ways to address this threat. On November 24 check out landmarks that will be lit blue to help increase visibility of AMR. Map here: https://caqd.short.gy/GoBlueforAMR
#GoBlueforAMR #WAAW2023
Suggested message #2.
Antimicrobial resistance (AMR) is one of the top global health threats, yet most don’t recognize its impact. #GoBlueForAMR is a colour campaign during World AMR Awareness Week to increase the visibility of AMR
Find out more: www.antimicrobialawareness.ca #WAAW2023
What is antimicrobial resistance (AMR)
Antimicrobials are medications designed to kill or stop the growth of microorganisms such as bacteria, viruses, fungi or parasites that cause infections. They include antibiotics, antivirals and antifungals used to prevent and treat infectious diseases in humans, animals and plants.
Antimicrobial resistance (AMR) occurs when bacteria and other microbes adapt in ways that allow them to fend off or disable antimicrobials. The microbes with ‘resistance’ survive and grow in number. This happens naturally, but overuse and misuse of antibiotics and other antimicrobials in humans and animals is increasing these changes, and faster than new antimicrobials come to market. The result is infections that are harder to treat, causing more severe illness, longer hospital stays, and more frequent death. In animals, AMR results in decreased animal health and welfare when these drugs are no longer able to treat these diseases.
This whiteboard video explains antimicrobial resistance and what it means to be a ‘steward’ of antibiotics.
Why does AMR matter to Canadians?
In Canada, a recent report estimated that 1 in 4 infections are already resistant to the first drugs used to treat them and 15 people die each day due to AMR infections.* Bacterial pneumonia, gonorrhea and urinary tract infections are some of the common infections that are becoming harder to treat. Without effective antibiotics, other treatments will also become risky. Patients needing surgery, dialysis and chemotherapy will be poorly protected from the risks of life-threatening infections.
*Download ‘When Antibiotics Fail’
What can you do to help address AMR?
- Use antimicrobials appropriately, only when and as prescribed. For example, do not use antibiotics for the cold, flu, or coronavirus infection.
- Do your best to prevent infections and stop them from spreading because fewer infections lead to less use of antimicrobials and less AMR. Keep vaccinations up-to-date, build healthy hand washing and food handling habits, and limit close contact with others during an illness.
- Dispose of antimicrobials properly. For example, return unused medication to a pharmacy, do not share antibiotics prescribed for you with others, or save them for later use.
Learn more from resources on this site developed by Canadian leaders in healthcare and antimicrobial stewardship.
PUBLIC RESOURCES

You can help combat antimicrobial and antibiotic resistance!
One of the most important drivers of antimicrobial resistance is the overuse of antibiotics. Become informed about appropriate antibiotic use and share the resources below. Learn from the personal stories of those harmed by drug-resistant bacteria and share their stories to make others aware of the human costs of antibiotic misuse and overuse.
Resources
Public Health Agency of Canada
Canada’s leading public health authority provides information on antibiotic resistance (and AMR), its causes, risks to human health, and the correct use of antibiotics. Learn how the Canadian government tracks and responds to this critical public health challenge.
AntibioticWise.ca
AntibioticWise provides videos and answers to your questions about antibiotics, their proper use, and antibiotic resistance. Learn about when and when not to use antibiotics.
Educator’s Resources
AntibioticWise provides lesson plans to help teachers, early childhood educators, public health nurses and other educators teach students about the basics of antibiotic resistance, germs, and the importance of handwashing.
Sometimes No Antibiotic is the Best Prescription
This short video for patients explores when you may not need antibiotics for upper respiratory tract infections and what you can do to feel better without antibiotics.
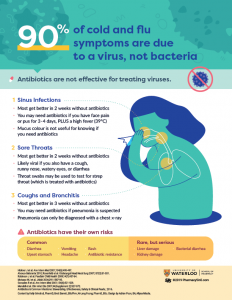
Antibiotics for cold and flu symptoms?
This handy infographic from the Pharmacy5in5 team at the University of Waterloo School of Pharmacy provides information on the appropriate use of antibiotics for common respiratory tract infections.
4 Common Infections – Do You Need Antibiotics?
Infographics from Public Health Ontario provide guidance on when antibiotics are not needed for some common infections. Topics include: Do you need antibiotics? Ear infection, Sinus infection, Sore throat, and Bronchitis.
Guide to Wise Use of Antibiotics
This guide, produced by Alberta Health Services’ Do Bugs Need Drugs program, helps you build knowledge on appropriate antibiotic use for your family. Learn what symptoms signal the need for medical attention and the best way to stop the spread of infections. Available in several languages, including four Indigenous languages.
Antibiotics and You
This video explains what antibiotics and the microbiome are, how they work, and the side-effects that you may experience. It also suggests questions to ask your healthcare providers when you have been prescribed an antibiotic.
Antibiotics and the Zoo Living In You
The microbiome is an important environment of trillions of organisms living on and within you. Watch this video to learn how antibiotics can disrupt this delicate ecosystem and what you can do to protect your microbiome.
Patients for Patient Safety Canada
The patient-led program of Healthcare Excellence Canada hosts a webpage in support of World Antimicrobial Awareness Week. Visit the webpage for patient stories and other resources developed specifically for patients and the public. Disponibles en français
Stories
What happens when antibiotics stop working?
Learn about the possible harms of drug-resistant microbes from those who have experienced an infection during a hospital stay, while traveling, or from an unknown source in their community.
Let these stories inspire you to learn and do more to use antibiotics and other antimicrobials wisely. Share them to help build awareness.
Mary’s Story
Mary’s story began with a post-surgical infection. Her experience reminds us that Canadians are at risk for resistant infections, and our older family members are vulnerable with extended use of antibiotics. Read her full story.
➤ SHARE her story: Facebook | Twitter | LinkedIn
Tatiana’s Story
Tatiana was a healthy 25-year-old newlywed when a resistant infection turned her life upside down. Read or watch her story of quarantine, many weeks of treatment, and long-lasting effects. This is one of many stories shared by the Antimicrobial Resistance Fighter campaign.
Kim’s Story
When her mother returned from hospital colonized by a drug-resistant organism, Kim looked for answers—what put her mother at risk, what now, and how could they help control the spread of a drug-resistant organism? ‘Drug-Resistant Infections – More than What Meets the Eye‘ is a patient perspective on AMR with tips for self-advocacy and infection prevention from Patients for Patient Safety Canada and the National Collaborating Centre for Infectious Diseases.
Vinesha’s Story
Cancer survivor Vinesha Ramasamy talks about the importance of antibiotics in this video produced by the Public Agency of Canada.
PROVIDER RESOURCES

Healthcare professionals are leaders for the appropriate use of antibiotics.
When the potential benefit of an antimicrobial outweighs the risk of harms, you and your team ensure patients get the right drug, at the right time, at the right dose, and for the shortest effective duration. Your actions promote quality patient care and protect public health.
Download and share tools and resources to help improve antimicrobial use and reduce harm to Canadians from antimicrobial resistance. Build knowledge of stewardship principles and their applications in practice through accredited training, accessible guidelines, and tips from experts.
Tools
Using Antibiotics Wisely Campaign
Choosing Wisely Canada provides practice change recommendations for primary care, hospital and long-term care settings. Resources are available—for primary care and long-term care settings. A third edition of the Cold Standard toolkit has been released for managing respiratory tract infections in the era of COVID-19 and virtual care.
Rethink Antibiotic Prescribing
Pharmacy5in5 is an online learning platform designed by pharmacists, popular for its innovative digital tools. Registration is open to pharmacy professionals in Canada. Check out their short video on antibiotic prescribing and related infographic.
Symptom-Free Pee: Let It Be
Help stop inappropriate antibiotic use for asymptomatic bacteriuria in long-term care residents and elderly patients in acute care. Download bilingual resources, freely available for use in your practice setting.
Viral Prescription Pads
To be used with patients who have a suspected viral infection, this time-saving educational tool provides information about symptomatic relief and indicates when to consider a return visit. Adult and child versions are available. Order free copies here.

Antimicrobial Stewardship Essentials
Practical, evidence-based information on how to promote antimicrobial stewardship in a range of healthcare settings, from Public Health Ontario. Learn more. NEW infographics on strategies to reduce antibiotic overuse in primary care.
Education & Guides
Bugs & Drugs – A Guide to Therapy
This comprehensive guide to antimicrobial therapy and aid to wiser antibiotic use in front-line practice is available as a mobile app for both Android and iPhone.
Community Antimicrobial Stewardship Continuing Education
A free, self-directed online course providing community-based practitioners with the latest evidence and treatment guidelines for use of antibiotics in primary care. Certified for 3.5 Mainpro+ credits.
Antimicrobial Stewardship Programs Chat (#ASPChat)
A real-time Twitter Chat promotes appropriate antibiotic use and stewardship in practice. Chats are open to all and run on the third Thursday of each month from 7-8 PM EST. Follow @ASP_chat for information.
Stories
Healthcare providers and public health leaders are witnessing the human and health system costs of antibiotic resistance, in Canada and around the world.
Their stories illustrate how important it is to adopt effective practices and policies. Read and share their stories to act on the threat of antibiotic and antimicrobial resistance.
The 7 Minutes
Prince County Hospital ER is a shining star on wise antibiotic use for the province of PEI. The 7 minutes spent explaining why a patient doesn’t need antibiotics is worth it. Watch it here.
You get the virus, you need a virus plan
Peters Wayne, Dr. Navqui and Greg Burton, community pharmacists from PEI, share their experiences with antibiotic prescription, advice to patients regarding antibiotic use, and antibiotic use in long-term care facilities. Watch it here.
Moxifloxacin
Sarah Lutes, a hospital pharmacist in PEI, shares her story about community acquired pneumonia (CAP) and how Health PEI’s development of guidelines helped to stop unwise prescribing of Moxifloxacin. Watch it here.
Keep Antibiotics Working
Pharmacist Christine Landry talks about the importance of responsible antibiotic use in this video produced by the Public Health Agency of Canada.
WEBINARS

Introducing the CAN AMS! Series
The Canadian Antimicrobial Stewardship Webinar Series
CAN AMS! is a new webinar series focused on antimicrobial stewardship (AMS) interventions. Leaders in AMS from across Canada share examples of what has been done to implement evidence-based interventions, with the goal to inspire what CAN be done to help slow the rise and spread of antimicrobial resistance (AMR).
The series aims to:
- highlight and build greater knowledge of evidence-based AMS interventions,
- help bridge knowledge gaps and capacity challenges that can limit the development of AMS interventions, and
- promote broad collaboration on AMS across regions, settings, and sectors.
CAN AMS! events promote a One Health frame for AMS to raise awareness for the interconnected drivers and consequences of AMR, and the need for shared solutions across human, animal, and environmental health domains.
UPCOMING WEBINARS
WEBINAR #1.
Three Can-Do Outlooks on AMS: A One Health Opener for the CANadian Antimicrobial Stewardship Series
Join this engaging session highlighting opportunities for antimicrobial stewardship (AMS) in human, animal, and environmental health domains. NCCID and AMMI Canada welcome leaders in AMS from across Canada for this launch of the ‘CANAMS!’ series. An opening address from the Public Health Agency of Canada will underscore One Health as the appropriate frame for responses to AMR and situate antimicrobial stewardship (AMS) with a high-level overview of the federal government-led Pan-Canadian Action Plan and priority actions. A panel discussion follows to shed light on different perspectives on AMS from stewardship leaders working in human, animal, and environmental health domains.
Date: April 22, 2024
Moderator: Yoav Keynan, MD, PhD
Speaker: Kanchana Amaratunga, MD, MPH, FRCPC, AMR Task Force, PHAC
Panelists:
Human Health – Lynora Saxinger, MD, FRCPC, CTropMed
Environmental Health – Ed Topp, PhD
Animal Health – J. Scott Weese DVM DVSc DACVIM FCAHS
WEBINAR #2.
Building an Antimicrobial Stewardship Committee in Long-term Care
Hold the Date: June 10, 2024
Details Coming Soon!
MORE TO COME
Coming events in the series will focus on antimicrobial stewardship in primary care in rural communities, lower-resourced acute care, and dentistry settings.
PAST WEBINARS
Check back for recordings, posted after each live event.
More Information:
- There is no fee to attend webinars, however, registration is required.
- Access instructions will be provided following registration.
- The program is not accredited.
- The virtual events will be delivered via ZOOM.
- Webinars will be delivered in English. To request materials available in French (e.g. slides or summaries) please contact nccid@umanitoba.canccid@umanitoba.ca.
- Webinars will be recorded and posted on this website and on NCCID’s YouTube account (@CentreInfection, Playlist: CAN AMS!)
CAN AMS! is co-hosted by the National Collaborating Centre for Infectious Diseases (NCCID) and the Association of Medical Microbiology and Infectious Disease Canada (AMMI Canada). The series is developed through the collaborative leadership of a national group of AMS stakeholders, the Network for Coordinated AMR Awareness, convened by NCCID.
MEDIA
ALLIED CAMPAIGNS
Join the global movement to stop Antimicrobial Resistance.
Fighting AMR is a global effort that requires collective action from all sectors of society. World AMR Awareness Week reflects this ‘One Health’ approach with multi-sector leadership from The Food and Agriculture Organization of the United Nations (FAO), the UN Environment Programme (UNEP), the World Health Organization (WHO) and the World Organisation for Animal Health (WOAH).
WAAW is celebrated annually from November 18th to 24th. Allied campaigns worldwide mark this week with activities to raise awareness of AMR and the need for more appropriate use of antibiotics and other antimicrobials.
Learn more from these leading campaigns:
ABOUT

Canadian collaborators promote a unified campaign and share leading resources
The National Collaborating Centre for Infectious Diseases (NCCID) convenes a network of leaders in antimicrobial stewardship program implementation and public or professional education in healthcare, academic institutions, government agencies, and community settings across Canada.
The partners collaborate to…
- align messages and extend the reach of a unified AMR awareness campaign during World AMR Awareness Week
- contribute to a set of leading resources and tools for the public and providers, shared on this website
- exchange information about successful approaches to building awareness and shifting behaviour toward improved use of antimicrobials in priority areas
See our list of partners listed below.
Contact
For more information, please contact the National Collaborating Centre for Infectious Diseases.
204-318-2591
Partners
![]()
antibioticwise.ca | @antibioticwise

antimicrobialresistancefighters.org | @AMResistance




choosingwiselycanada.org | @ChooseWiselyCA
dobugsneeddrugs.org | @DoBugsNeedDrugs
firstline.org/ambassador | @Firstline

healthcarecan.ca | @HealthCareCAN
healthcareexcellence.ca | @HE_ES_Canada

horizonnb.ca | @HorizonHealthNB



patientsafetyinstitute.ca | @patients4safety
![]()
canada.ca | @GovCanHealth and @CPHO_Canada

publichealthontario.ca | @PublicHealthON

qualityofcarenl.ca | @QualityofCareNL

saskhealthauthority.ca | @SaskHealth

antimicrobialstewardship.com | @SHSUHNASP
uwaterloo.ca/pharmacy | @UWPharmacy and @pharmacy5in5
Production of this website has been made possible through a financial contribution from the Public Health Agency of Canada. The views expressed herein do not necessarily represent the views of the Agency.